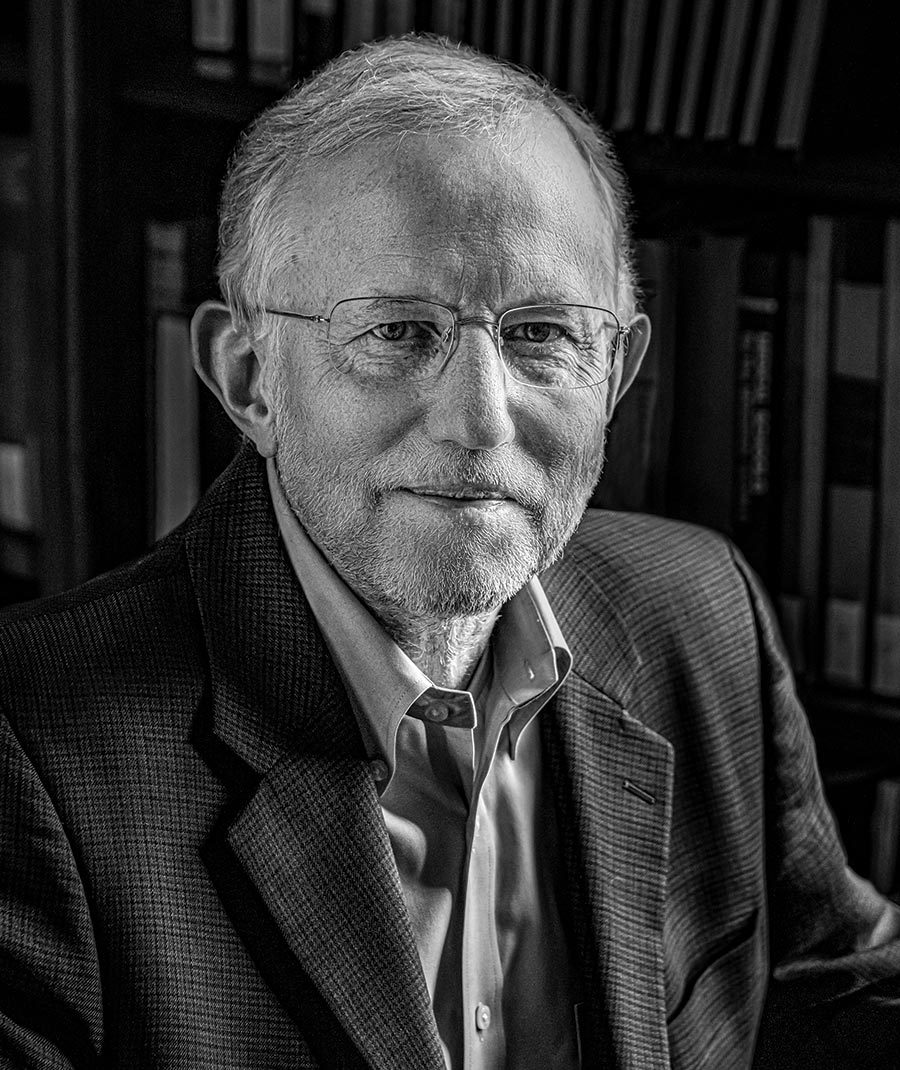

“A voice speaking with a Swedish accent introduced himself as the secretary of the Nobel Committee, and congratulated me on the prize, which I had been awarded together with Harvey Alter and Michael Houghton for the discovery of hepatitis C virus. This did begin to sound like it wasn’t a crank phone call or joke. I didn’t really get back to sleep after that,” Rice said. I recently talked to Rice, now the Maurice R. and Corinne P. Greenberg Professor in Virology at The Rockefeller University, about his time at UC Davis and his Nobel-winning work.
How did it feel to get the call about the Nobel Prize?
It was a total surprise, and it still is. It is humbling and a bit embarrassing to be singled out for something like this when so many people have contributed to this success story throughout the world both on the basic science side, the clinic, and in biotech and pharma to really get these remarkable new treatments to the finish line. I hope that the public appreciates what science can bring and that we’ll see another example soon for SARS-CoV-2 and COVID-19.
What was the first thing you did after the call?
I made a pot of coffee, I took a shower and decided I better put on a shirt with a collar … he warned me that somebody from the press was going to be calling in about half an hour and that at about 5:30 a.m. on the East Coast or I guess 11:30 a.m. in Sweden the formal announcements would be made. I could go ahead and log into the Nobel website and then watch this, which I did.
Going back to your time at UC Davis, you started there in 1970. What were you hoping to study?
I was pretty unfocused. When I showed up there as a freshman I actually didn’t even declare a major until we were told several years later that we had to have a major in order to graduate. At that point I went through the courses I’d taken and zoology won out. It was really the introductory biology course at Davis that got me interested in biology, and I also connected with the instructor, Dennis Barrett, who turned out to be very influential in my career trajectory. [Barrett] was a developmental biologist who worked on sea urchins at the Bodega Bay marine station. He was doing in vitro fertilization, and you could watch these incredible developmental events taking place under the microscope — really quite captivating. I recall having some wonderful trips to the Bodega marine station to work on the sea urchins. This really got me interested in developmental biology.
What memories stand out from your time at UC Davis?
There was a real presence of genetics at Davis in the ’70s, incredible evolutionary geneticists like Theodosius Dobzhansky and G. Ledyard Stebbins and a raging controversy between the theory of evolution and the special creationists. I can remember amazing encounters between Stebbins and Duane Gish debating these topics to packed audiences in Freeborn Hall. It was a fascinating time and a formative one for me. In terms of the UC Davis campus I still remember good times hanging out on the Quad, and I loved the college town atmosphere where you could get around easily on a bicycle just about anywhere you would want to go. I really enjoyed campus life.
You took a gap year after graduating?
With a couple of friends from Davis I bought a clunky Volkswagen van and headed off driving through Mexico, Guatemala and Central America. My friends came back at that point, and I went on to Colombia, Ecuador, Peru, Bolivia, Argentina, and I had a wonderful time. I was actually in Lima, Peru, when I got a telegram from my dad — this was well before email and cell phones — stating that I had received a letter from Caltech where I applied to graduate school. They needed to know if I was actually going to come or not. I decided at that point that it might be good to transition back from being a vagabond. Perhaps the experience that really convinced me that I wanted to do research was taking the physiology course at the Marine Biology Laboratory in Woods Hole, Massachusetts, the summer before my last year at Davis. And again, Dennis Barrett was a player in that because he was an instructor in the course and probably had a lot to do with an undergraduate being admitted. It was just an amazing experience. So I did that in 1973, the summer between my junior and senior years, and then I actually went back there in the summer of 1975 as a TA after returning from South America. This turned out to be a good means of transitioning from traveler to graduate student. Caltech was where Dennis Barrett had gone to graduate school, and there was a world-class lab there studying sea urchin development. But when I ended up at Caltech, I found myself in Jim and Ellen Strauss’ lab studying this model enveloped RNA virus called Sindbis virus. So this random event of unexpectedly getting into a molecular virology lab turned out to be what I ended up doing for my entire career.
Did not making it into the development lab disappoint you?
This was something that was new to me, and interesting. I think it shows that I tend to get interested in just about anything. I have to admit that the virus angle — working with a relatively simple entity that you can manipulate genetically, and also use to study how it effects cell biology — was just very attractive and still is.
Turning to your hepatitis C work, after Caltech you had moved to Washington University in St. Louis working on yellow fever virus, which belongs to the same family as hepatitis C virus. How did you get involved?
In 1989, I got a phone call from Steve Feinstone [at the Food and Drug Administration]. We had sequenced the vaccine strain of yellow fever virus, called 17D, and established an infectious clone. That meant we could manipulate the genome and look at the effects of those mutations on the virus life cycle. In the last sentence of our paper we suggested the use of 17D as a vehicle for other vaccines. Steve called me up out of the blue and said, “Hey, Charlie, how about making a yellow fever 17D/HCV chimera as a vaccine?” We got to talking but then realized we really knew very little about the hepatitis C genome and how the viral proteins were expressed.
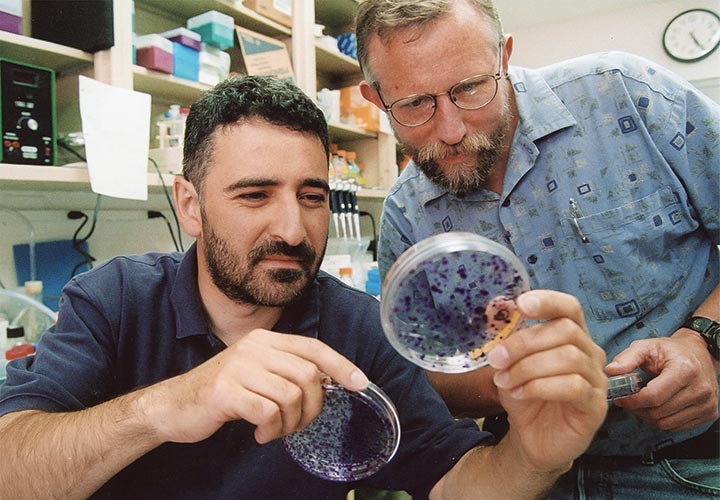
You mentioned that hepatitis C virus is very difficult to grow in culture.
People had been trying to amplify this virus in culture by taking isolates from patients and dumping them on various cell types, but this had failed miserably. Based on sequences published in 1989 and shortly thereafter, there were also numerous attempts to construct infectious HCV cDNA clones that could be used to launch virus infection. These attempts had also failed. When we sequenced the genome of the yellow fever virus, it ended with what turned out to be a very stable stem loop RNA structure so we began wondering if this wasn’t also the case for hepatitis C virus. We discovered a structure of about 100 bases at the end of the genome that had been missed that was simultaneously found by Kunitada Shimotohno’s lab in Japan. We thought with this missing piece we should be able to get a replication competent, infectious HCV RNA from cloned cDNA. However, the only way we could test this was the chimpanzee model, so with Steve Feinstone’s group we injected RNA into the liver of chimps and again failed to detect virus. We still weren’t there. We knew the virus was very error prone. You have a trillion variants being generated per day in a single chronically infected individual — some of those mutations are lethal [i.e., the virus won’t grow]. The solution we came up with was to construct a consensus sequence. Alexander “Sasha” Kolykhalov assembled a library of clones of different variants and painstakingly went through and assembled a consensus sequence [where most of the sequences were in agreement for each letter]. When these consensus sequences were tested in two chimpanzees by Steve and his team there was finally evidence of hepatitis C virus RNA in circulation. That was really the moment when we had molecular proof of Koch’s postulates, that you’ve isolated and purified the disease-causing agent, and when it’s introduced back into a susceptible host it is sufficient to cause infection and disease. We finally also had a functional, viable HCV genome sequence.
You won the Nobel Prize for your work in hepatitis C, and you’ve now turned to work on COVID-19?
When a new virus genus pops up it can be irresistible for virologists to study. We were already taking a look at what was happening in January [2020] with the emergence of this virus, looking at the rapid spread and wondering if we would have a pandemic on our hands. We had started work on coronaviruses from another angle about two years before with a group in Switzerland to see if we could understand more about how interferon could exert a protective effect against seasonal coronaviruses as well as SARS-CoV and MERS. We were about to publish a paper on this in January 2020 when SARS-CoV-2 showed up. We quickly confirmed that [the interferon effect] was also the case for SARS-CoV-2. I think the progress that’s been made is amazing. I know the general public thinks that one should be able to identify the virus and figure everything out in a few days, but unfortunately things don’t work like they do in Hollywood movies so it’s taking a little bit longer. But as I look at it, from the discovery of hepatitis C in 1989, the development of tools for drug discovery and finally the new classes of potent antiviral drugs — this took more than 25 years of really hard work. I do think we’re on a trajectory with SARS-CoV-2 and COVID-19 that is about 20 times faster than our experience with hepatitis C virus. I’m very optimistic that we’re going to be able to get this under control in record time. One of the things that I think will come out of this are some potent new drugs to treat infections, but also we’re going to really learn a lot about vaccine technology. I think that is going to have a lasting contribution for future vaccine efforts.